
Discover the rich western heritage and unique appeal of Fort Worth.
Fort Worth is “The Unexpected City”. The nation’s 13th largest city has a rich western heritage and is home to world-class museums, top hotels and restaurants, a 35-block entertainment district in downtown, and unique meeting venues. Here are the top six reasons you’ll boost your attendance by meeting in Fort Worth, the fastest growing city in the U.S.
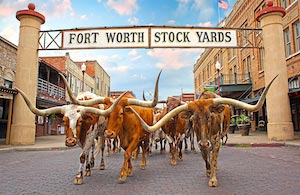
World’s Only Twice-Daily Cattle Drive
Watch cowhands drive a herd of Texas longhorns down East Exchange Avenue in the Stockyards National Historic District for a glimpse of life in the Old West. The Stockyards is the most visited Western Heritage District in America.

5 Connected Museums
There’s a reason Fort Worth is called “the museum capital of the Southwest.” The Cultural District boasts some of the finest museums in the U.S. Five of the best are in a single, park-like setting. Take in masterpieces from priceless antiquities to modern gems.
10 Minute Town
You don’t have to go too far in Fort Worth. Ten minutes from downtown you can explore 18 districts, including Clearfork, where there’s no shortage of great places to eat, nightlife, and shopping. There’s Riverside with its park tucked between Trinity River and Oakhurst Scenic Drive; and the Northside, with the Rose Marine Theater that hosts Hispanic arts, the National Multicultural Western Heritage Museum and Marine Park, one of the oldest parks.


#2 Zoo in the Nation
The Fort Worth Zoo has more than 500 species of animals and $100 million in new exhibits.
Getting to and Around Fort Worth is Easy
The Dallas Fort Worth International Airport has the most nonstop flights that go anywhere in the U.S. in four hours or less. The free downtown trolley serves downtown hotels, attractions, and the convention center.


Abundance of Accommodations
There are more than 4,000 hotel rooms in downtown.
Learn more here about planning your next meeting in Fort Worth.
